References:
- Boe NJ, Hald SM, Jensen MM, Kristensen LMB, Bojsen JA, Elhakim MT, Clausen A, Möller S, Hallas J, García Rodríguez LA, Selim M, Goldstein LB, Al-Shahi Salman R, Gaist D. Major Cardiovascular Events After Spontaneous Intracerebral Hemorrhage by Hematoma Location. JAMA Netw Open. 2023 Apr 3;6(4):e235882. doi: 10.1001/jamanetworkopen.2023.5882. PMID: 37017964; PMCID: PMC10077102.
- Li L, Murthy SB. Cardiovascular Events After Intracerebral Hemorrhage. Stroke. 2022 Jul;53(7):2131-2141. doi: 10.1161/STROKEAHA.122.036884. Epub 2022 Jun 8. PMID: 35674043; PMCID: PMC9247019.
- Li L, Poon MTC, Samarasekera NE, et al. Risks of recurrent stroke and all serious vascular events after spontaneous intracerebral haemorrhage: pooled analyses of two population-based studies. Lancet Neurol. 2021;20(6):437-447.
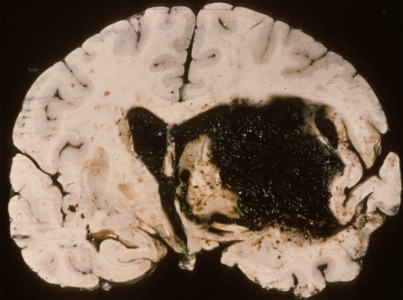
We know that stroke workups can sometimes make you feel like your brain is hemorrhaging, but let’s keep that figurative, shall we? Turning our attention to actual intracerebral hemorrhages (ICH), a comprehensive study from The Lancet Neurology offers illuminating insights. With an eye on long-term outcomes, this study focuses on recurrent ICH rates, ischemic stroke incidence, and other serious vascular events. Here’s what you should know…
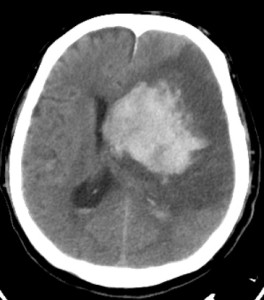
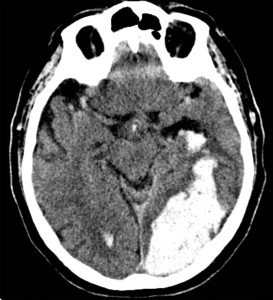
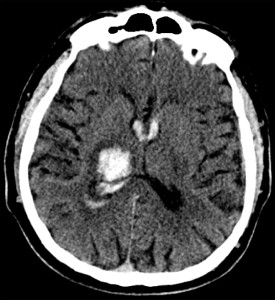
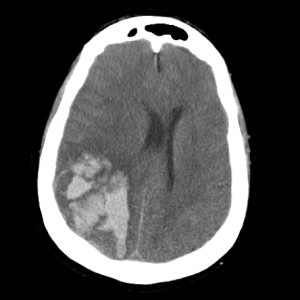
The study is a pooled analysis from the Oxford Vascular Study (OXVASC) and the Lothian Audit of the Treatment of Cerebral Haemorrhage (LATCH). It analyzed 674 first-time ICH patients over 1553 person-years. The cohort’s mean age was 74.7, 47% were male, and 51% were on antithrombotics before their ICH. Additionally, 22% had atrial fibrillation, and 47% had lobar ICH while the rest had non-lobar ICH.
The recurrent ICH rate was 3.2 per 100 person-years based on 46 events in the cohort. The ischemic stroke rate was 1.7 per 100 person-years from 25 events, and the rate for any serious vascular event was 7.9 per 100 person-years from 118 events. Lobar ICH had a higher risk of recurrent hemorrhage with a hazard ratio (HR) of 3.2 (95% CI 1.6-6.3; p=0.0010). Ischemic stroke risk was not location-dependent with an HR of 1.1 (95% CI 0.5-2.8; p=0.76). Atrial fibrillation at the time of the initial ICH increased ischemic stroke risk significantly (HR 8.2, 95% CI 3.3-20.3; p<0.0001).
The study accentuates the importance of two critical risk-stratification parameters for post-ICH management: the anatomical location of the hemorrhage and the presence of comorbid atrial fibrillation. The anatomical location, specifically whether it’s lobar or non-lobar, can be a predictive factor for the likelihood of recurrent hemorrhages. Conversely, atrial fibrillation is a crucial determinant for assessing the heightened risk of ischemic stroke. These risk stratification elements not only lend support to the findings of the RESTART trial but also underscore the urgency for specialized clinical trials that aim at targeted interventions for high-risk subgroups.
In light of recent research, risk stratification in post-ICH management becomes even more critical. A Danish study with 2,819 patients reinforced the Lancet’s findings, showing higher recurrent lobar ICH rates of 3.74 per 100 person-years with an adjusted HR of 2.63 (95% CI 1.97-3.49). The same study emphasized a higher absolute rate of major cardiovascular events (the aggregate of intracerebral hemorrhage, ischemic stroke, non-traumatic extracranial bleeding, myocardial infarction, systemic thromboembolisms, or death due to vascular causes) and myocardial infarctions in non-lobar ICH for those with atrial fibrillation. Another review reported ischemic stroke rates of 3-7% and myocardial infarctions around 4% post-ICH. These recent insights collectively underscore the dire need for targeted clinical trials, particularly involving antithrombotics and statins, to improve secondary prevention strategies in ICH care.
Feel free to review the original article yourself here!
Check out some relevant images from our website below: