Below you will find over 50 EMG/NCS Practice Cases! Each electromyography/nerve conduction study case has associated clinical presentations and a brief explanation of the diagnosis. Note not all cases will have both EMG and NCS data.
Please note that this chapter does not cover how to interpret an EMG/NCS study. Before reviewing this section it would be wise to read our EMG/NCS Chapter. It will provide you with the foundation to help you interpret these EMG/NCS Practice cases. If you are curious about what some of these EMG findings look like on recording check out our EMG Video Gallery. It is important to be able to interpret NCS and EMG studies on both the RITE and ABPN neurology board exams. Review and repetitive practice are key!
Acronyms/abbreviations:
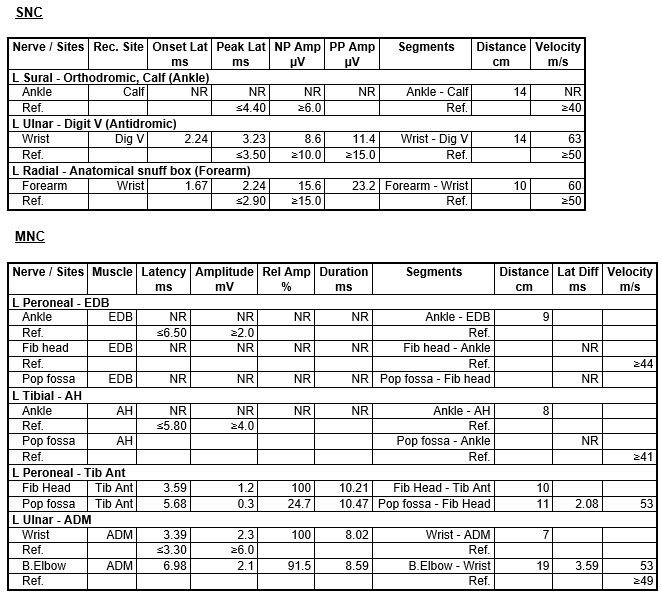
- IA: Insertional activity, Fib: Fibrillations, PSW: Positive spike waves, Fasc: Fasculations, MUAP or MUP: Motor unit action potential, Dur.: Duration, Amp: Amplitude, PPP: Polyphasic potentials, Rec. Site: Recording Site, NR: No Response, NP Amp: Negative peak amplitude, PP Amp: Peak-to-peak amplitude.
- 1+, 2+, 3+, 4+: The degree of finding severity (1 is minimal, 4 is maximal).
- N: Normal, Sl Incr: Slightly increased, Gr Incr: Greatly increased, Mod: Moderate.
Table of Contents
Motor Neuron Disease
Case 1
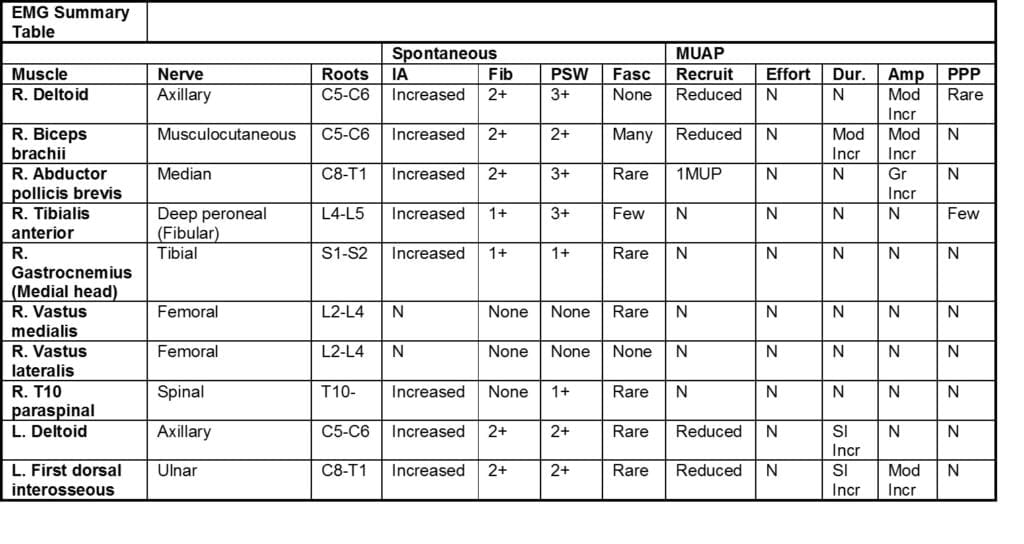
A 63-year-old male presents with progressive muscle wasting and diffuse atrophy:
This abnormal study provides electrodiagnostic evidence of widespread acute and chronic denervation affecting lumbosacral, thoracic, and cervical myotomes. These findings meet El Escorial criteria for ALS.
Case 2
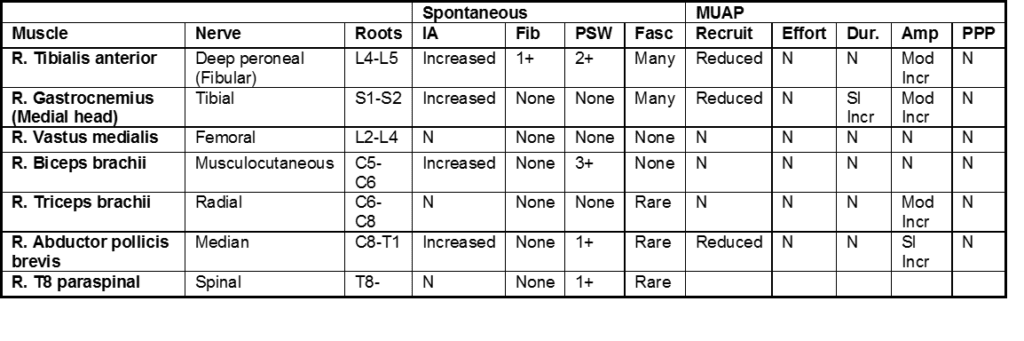
Patient is a 75-year-old male with a past medical history of Lewy body dementia, referred by his cognitive specialist for evaluation of lower extremity fasciculations
This was an abnormal study, with electromyographic findings that meet Awaji criteria for amyotrophic lateral sclerosis (ALS).
Case 3
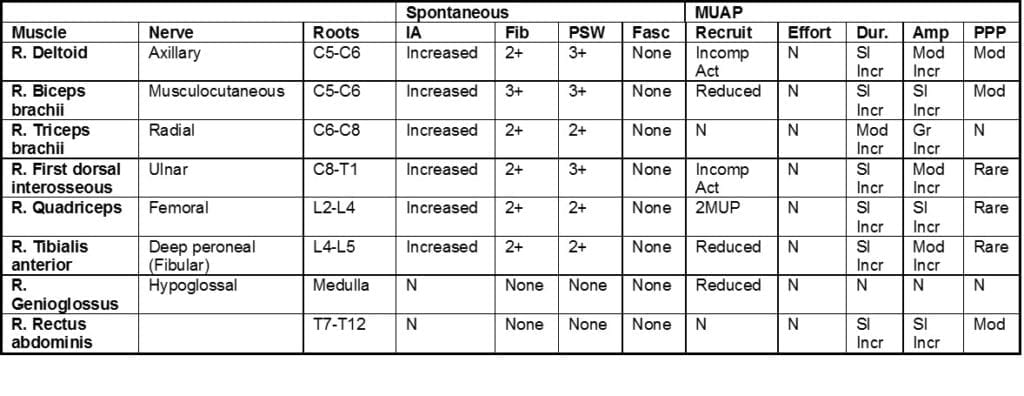
This 49-year-old female has had pain in her neck area and has been losing weight recently. On examination there is generalized muscle loss.
This is an abnormal study, with electrodiagnostic evidence of widespread acute and chronic denervation in cervical and lumbosacral-innervated muscles which supports a diagnosis of motor neuron disease.
Case 4
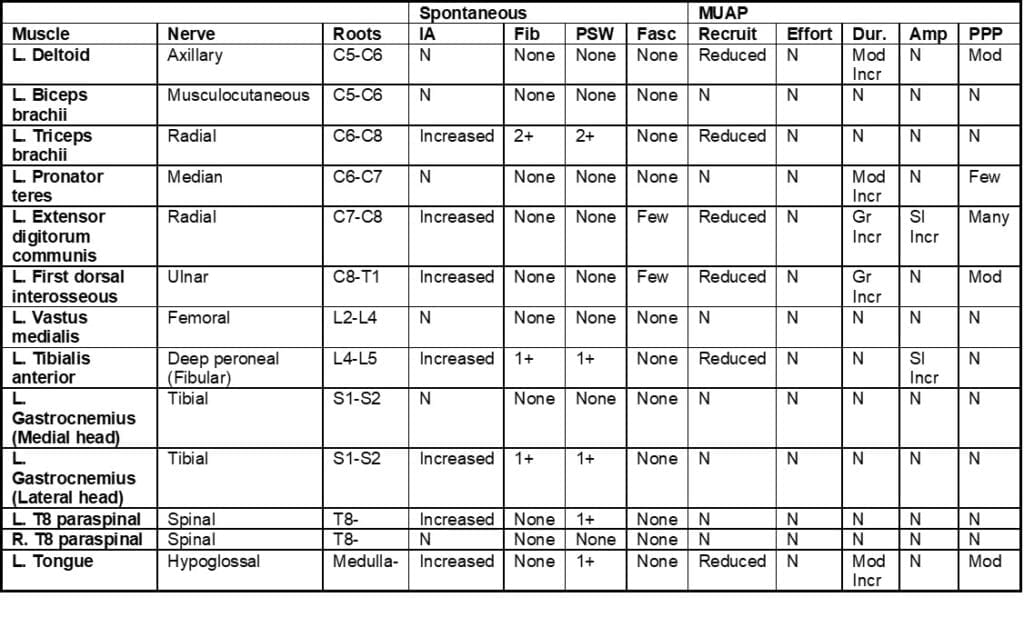
The patient is a 64-year-old woman who is referred to the EMG lab for assessment of bilateral hand weakness for the past 6 months.
This abnormal study shows evidence for chronic neurogenic changes in the tongue, the thoracic paraspinal muscles and in several muscles of the arm and leg. These changes meet the El Escorial criterion for ALS.
Hereditary Neuropathies
Case 1
The patient is a 31 year old female with a history of Charcot Marie Tooth (CMT).
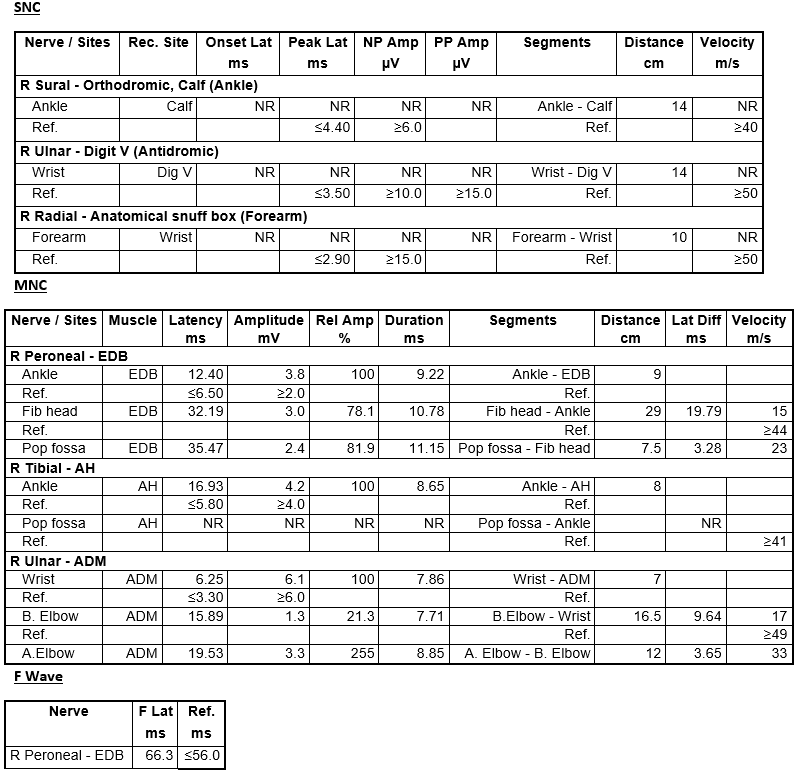
This is an abnormal study, with electrodiagnostic evidence of a sensorimotor demyelinating polyneuropathy. Active axon loss is not found, but chronic denervation is recorded in distal muscles of the leg. These findings are most consistent with a CMT1A gene mutation.
Case 2
Patient is a 48 year old male with a history of lower extremity weakness:
This is an abnormal study with electrodiagnostic evidence of moderate length-dependent sensorimotor dysmyelinating polyneuropathy. These types of findings are most commonly seen in patients with CMT1A phenotypes.
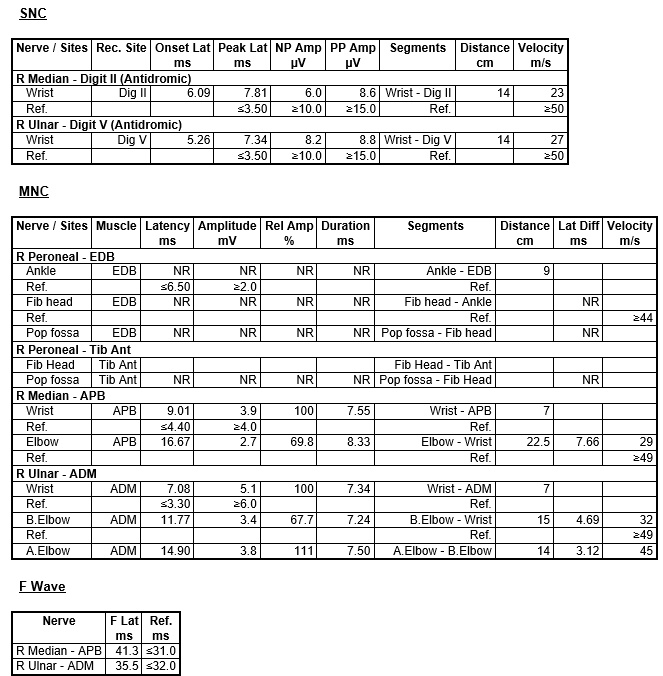
Case 3
61-year-old female referred for evaluation of CMT:
This is an abnormal study with electrodiagnostic evidence of sensorimotor mixed polyneuropathy with uniform slowing. This pattern of neuropathy can be seen with hereditary neuropathies like CMT1X, CMT1B and 1A.
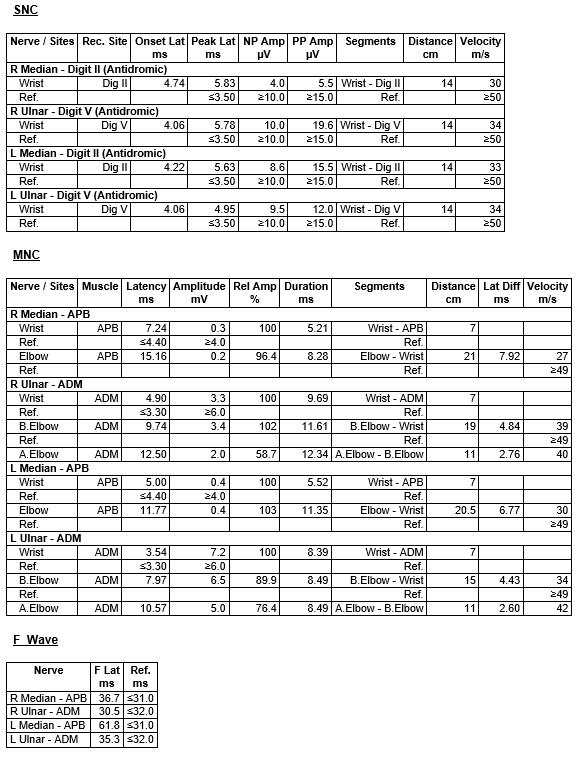
Case 4
The patient is a 71 year old male with a history of mild ankle weakness and balance issues for the last 6 years. A few of his siblings and father had the same symptoms. On exam he has high arches and hammertoes.
This EMG showed evidence of a severe sensorimotor axonal polyneuropathy. EMG showed evidence of acute and chronic denervation. Given his exam and family history, this is most likely an inherited neuropathy, likely CMT type 2.
Case 5
The patient is a 56 year old female with painful paresthesias for the last several years. She endorses a family history of similar symptoms in many family members.
This is an abnormal study with electrodiagnostic evidence of severe, axonal, length dependent sensorimotor polyneuropathy. Given the prominence of family history, these findings are suggestive of genetic polyneuropathy, such as CMT type 2.
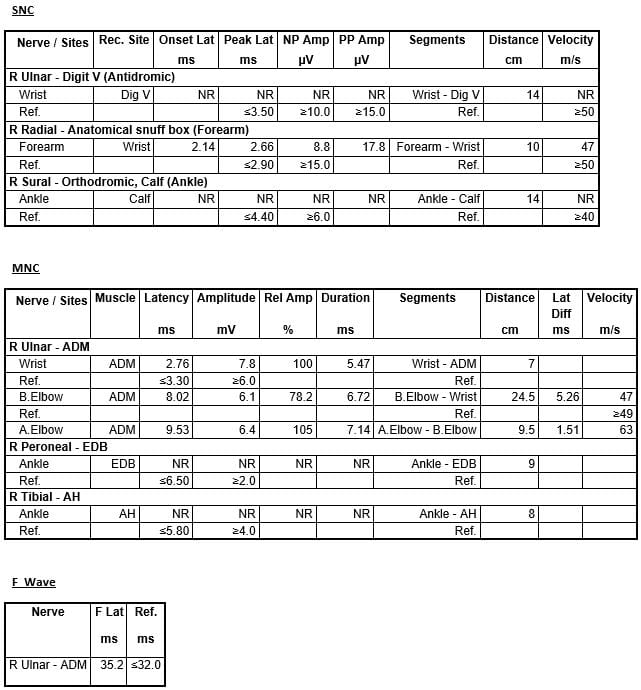
Mononeuropathies
Upper extremity
Log in to View the Remaining 60-90% of Page Content!
New here? Get started!
(Or, click here to learn about our institution/group pricing)1 Month Plan
Full Access Subscription-
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
3 Month Plan
Full Access Subscription-
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
1 Year Plan
Full Access Subscription-
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content