Vascular neurology requires an understanding of both neuroanatomy and vessel anatomy, as well as knowledge of up-to-date treatment protocols. This chapter review encompasses the pertinent information to excel with neurology exams. Real MRI, angiography, and gross specimens are available to aid in your study, and you may test your knowledge with our Question Bank and flashcards at the end!
Authors: Bradley Klein MD, Brian Hanrahan MD, Pouria Moshayedi MD
Transient ischemic attack (TIA)
- Defined as a transient episode (<24 hours) of neurologic dysfunction caused by focal ischemia, without acute infarction.
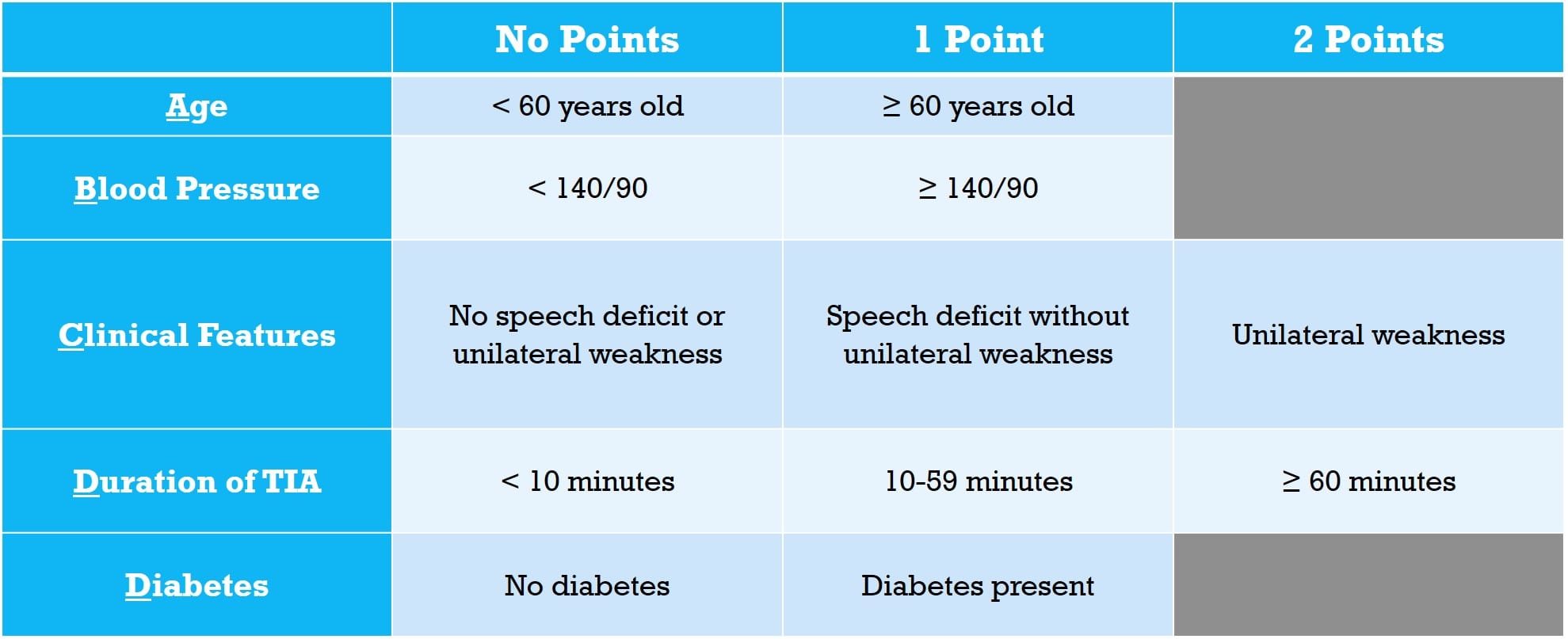
- ABCD2 score is used to predict 7-day risk for stroke after TIA.
- 7-day risk of stroke based on ABCD2 score:
- 0-3 points: 1.2%
- 4-5 points: 5.9%
- 6-7 points: 11.7%
Please Note
The ABCD2 score does not take into account severe carotid or intracranial stenosis which is also a risk for ischemic stroke after TIA
Exam Tip
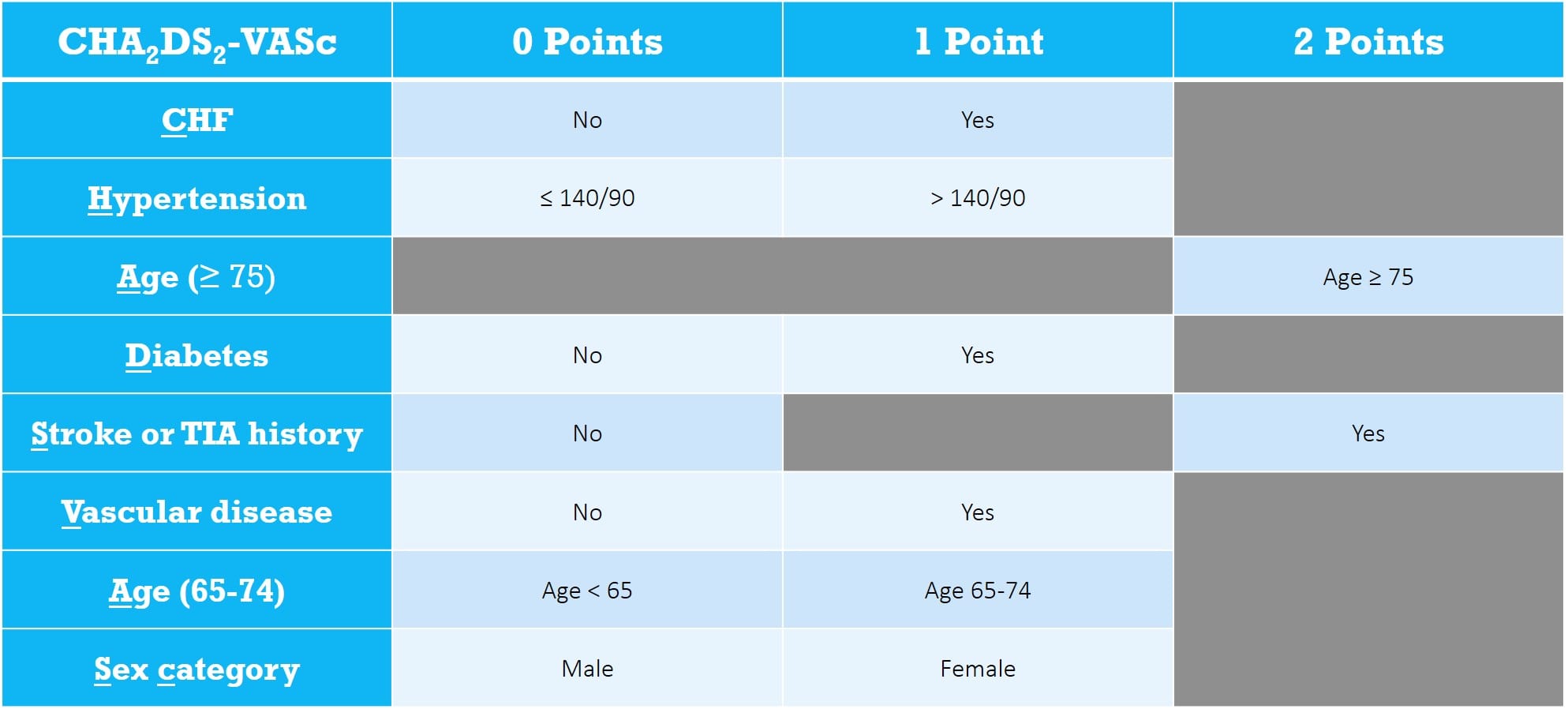
This chapter contains three different scores (ABCD2, HAS-BLED, & CHA2DS2-VASc). It would be very unusual for an exam to ask you to calculate a numeric score. Rather, they are much more likely to simply ask you to name the risk variables used for that score (the far left column).
Ischemic stroke
Stroke subtypes (by TOAST criteria)
Large-artery atherosclerosis
- The most common cause of ischemic stroke in the world.
- Patients will have either significant stenosis or occlusion of a major brain artery or branch cortical artery.
- Symptomatic Carotid: Stenosis of the common carotid ipsilateral to a TIA or infarct.
- Carotid endarterectomy (CEA) or carotid artery stent (CAS) is indicated if the stenosis is 50-99% in men or 70-99% in women.
- Asymptomatic carotid stenosis should be treated surgically if the stenosis is 80-99%.
- CEA has a higher risk of periprocedural myocardial infarction
- CAS has a higher risk of periprocedural stroke
- Treatment with CEA or CAS can lead to cerebral hyperfusion syndrome, which presents with headaches, visual disturbances, and seizures.
- Occurs secondary to dysautoregulation of cerebral vessels in regions which been in chronic low-flow states.
Cardioembolism
- The most common cause of ischemic stroke in the United States.
- Patients can present similarly with comparable imaging to those with large-artery atherosclerosis but will have a cardiac source for the embolic phenomenon.
- Sources of cardioembolism: Atrial fibrillation, mechanical heart prosthetic valve, left atrial or ventricular thrombus, recent myocardial infarction, dilated cardiomyopathy, valvular heart disease, structural heart defects, tumors, etc.

- The CHA2DS2-VASc Score helps to calculate the risk of stroke in patients with untreated atrial fibrillation.
Lipohyalinosis/small-vessel disease
- Commonly occurs in the lenticulostriate vessels of deep cortical structure.
- Also known as lacunar strokes, these are felt to be related to chronic hypertension, diabetes, and smoking.
Stroke of Other Determined Etiology
Hypercoagulability and coagulopathy
- Examples: Factor V Leiden, antiphospholipid antibody syndrome, protein S/C deficiency, prothrombin gene mutation, antithrombin III syndrome, sickle cell disease, thrombotic thrombocytopenic purpura (TTP), polycythemia, hyperhomocysteinemia, MTHFR gene mutations, and malignancy.
- Blood transfusions can decrease the risk of stroke in patients with sickle cell disease.
- More likely to cause venous events than arterial.
- Examples: Factor V Leiden, antiphospholipid antibody syndrome, protein S/C deficiency, prothrombin gene mutation, antithrombin III syndrome, sickle cell disease, thrombotic thrombocytopenic purpura (TTP), polycythemia, hyperhomocysteinemia, MTHFR gene mutations, and malignancy.
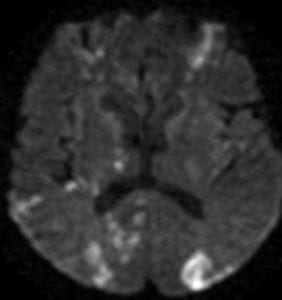
Central nervous system (CNS) vasculitis
- CNS vasculitis is a syndrome caused by a diverse spectrum of diseases that typically involves the gray/white matter junction.
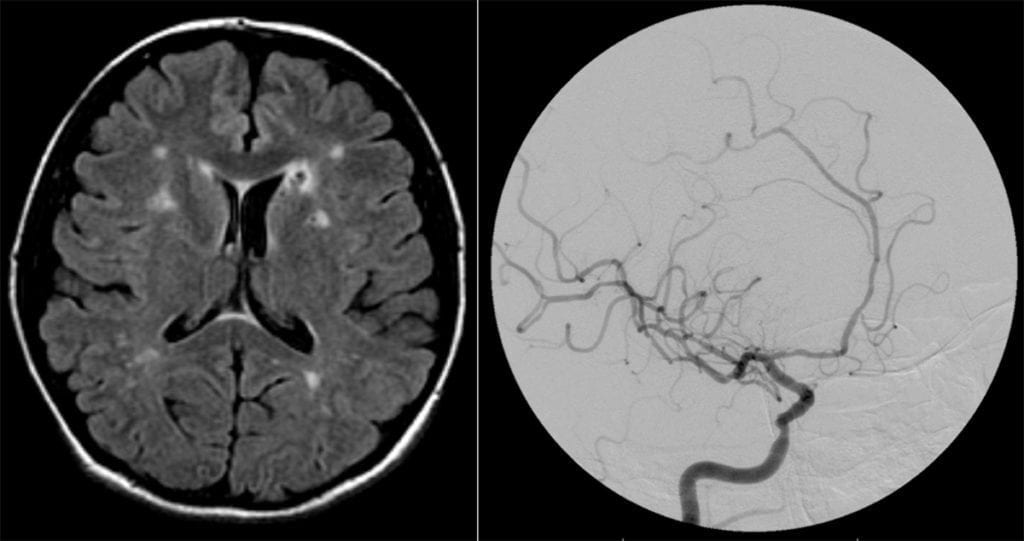
- Diffusion-weighted sequences on MRI will show multiple small focal areas of acute infarction in multiple vascular territories.
- Vessel imaging will show marked beading and segmentation alongside numerous arterial structures.
Primary CNS Vasculitis
- Primary angiitis of the CNS (PACNS):
- Vasculitis confined only to the small-medium sized blood vessels in the brain, spinal cord, and meninges.
- Primary angiitis of the CNS (PACNS):
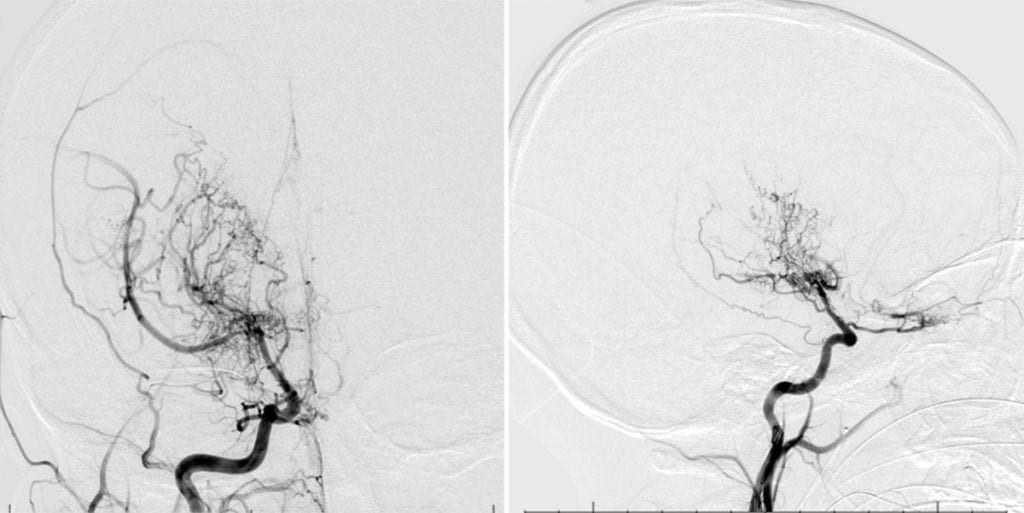
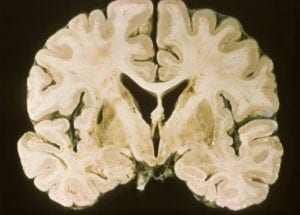
Moyamoya disease
- Congenital Moyamoya disease is seen most often in patients of Asian descent.
- Mysterin/RNF213 as a susceptibility gene for congenital moyamoya.
- Secondary causes of Moyamoya disease include head/neck radiation, sickle cell disease, neurofibromatosis, and prothrombotic disorders.
- Angiogram will show an abnormal vascular pattern of small net-like lenticulostriate vessels characterized as a “puff of smoke” with severe stenosis or occlusion of the distal internal carotid arteries.
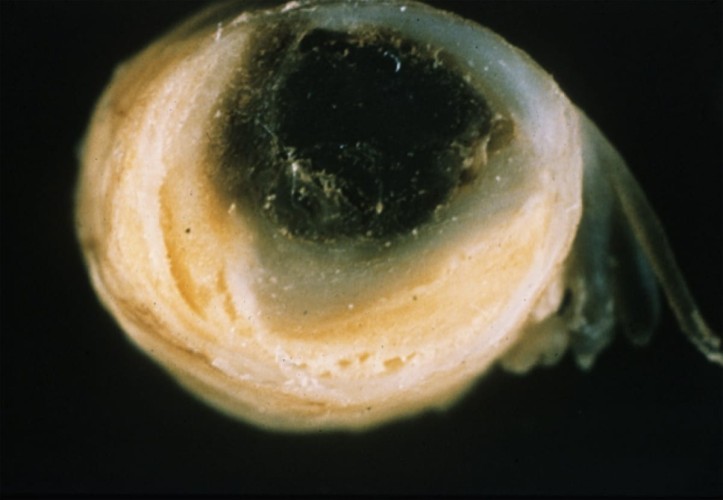
Moyamoya Disease - Pathology:
- Large vessel thickening of the intima, small overgrown dilated small arteries, and regions of ischemic and/or hemorrhagic infarct.
- Congenital Moyamoya disease is seen most often in patients of Asian descent.
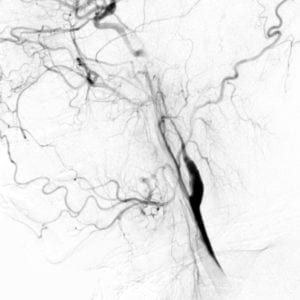
Arterial dissection
- Dissections are due to a tear of the vessel wall intima leading to a formation of a false lumen.
- Symptoms can include head/neck pain and Horner syndrome. Ischemic events occur due to thromboemboli formation and less often cerebral hypoperfusion.
- A common cause of stroke in the young. Should be considered in a patient with a history of neck trauma, chiropractic neck manipulation/high-velocity neck injury, or connective tissue disease (fibromuscular dysplasia, Marfan syndrome, Ehlers-Danlos syndrome).
- Dissections are often extracranial and vessel imaging may show a “string sign” or flame-shaped occlusion in the area of the dissection.
Right ICA Dissection
Patent foramen ovale (PFO)
- Seen in roughly 20% of people and its presence alone is not a strong risk factor for ischemic stroke. PFO’s shouldn’t be considered as an etiology for stroke unless a patient presents with a cryptogenic embolic stroke.
- Lesions that are large, have a significant right to left shunt or are accompanied by an atrial septal aneurysm have a higher risk of recurrent stroke.
- While the standard of care for secondary stroke prevention in those with PFO is antiplatelet therapy, recent data suggest that surgical PFO closure for those with high-risk features reduces the risk of recurrent stroke, and should be considered if the patient is <60 years of age.
- PFO closure in young stroke patients decreases the risk of secondary stroke.
- Seen in roughly 20% of people and its presence alone is not a strong risk factor for ischemic stroke. PFO’s shouldn’t be considered as an etiology for stroke unless a patient presents with a cryptogenic embolic stroke.
Air embolus
- The entry of air into the vasculature can be related to surgery, trauma, intravascular catheters, and barotrauma.
- If CTH is performed promptly after insult, air can be seen within the cerebral vessels.
- Treatment includes emergent use of a hyperbaric oxygen chamber, but the prognosis is often poor.
Fat embolism syndrome (FES)
- FES occurs secondary to long bone or pelvic fractures leading to the release of fatty bone marrow into the systemic circulation.
- Emboli obstruct pulmonary arteries leading to respiratory distress. Microemboli can pass through the pulmonary circulatory system and extend into the systemic arterial system and brain leading to small, randomly distributed ischemic strokes.
Hypoperfusion
- Hypoperfusion can cause watershed regions between major vascular territories to become ischemic.
- Imaging will show ischemia along border zone regions of the ACA-MCA and MCA-PCA territories.
- Bilateral ACA-MCA border zone infarcts can cause “man in the barrel” syndrome: upper extremity paralysis with retained strength in lower extremities.
- Bilateral MCA-PCA border zone infarcts can cause Balint’s syndrome: the triad of simultagnosia, oculomotor apraxia, and optic ataxia.
Border zone Infarcts
Mitochondrial Encephalopathy, Lactic Acidosis, and Stroke-like episodes (MELAS)
- MELAS is a mitochondrial disease caused by a mitochondrial DNA mutation to the gene MT-TL1.
- Symptoms of ischemic strokes, seizures, and headaches present before the age of 40.
- Diagnostic testing will reveal elevated cerebral spinal fluid lactate levels, serum lactic acidosis, and ragged red fibers on muscle biopsy
Trauma
Drugs/Toxins
- Common drugs that induce stroke include cocaine and amphetamines.
Stroke of Undetermined Etiology
- A diagnosis that is given to patients in which a cause of a stroke cannot be determined with any degree of confidence.
- Many patients with stroke of undetermined etiology will ultimately be found to have paroxysmal atrial fibrillation with prolonged heart monitoring.
Log in to View the Remaining 60-90% of Page Content!
New here? Get started!
(Or, click here to learn about our institution/group pricing)1 Month Plan
Full Access Subscription
$142.49
$
94
99
1 Month -
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
3 Month Plan
Full Access Subscription
$224.98
$
144
97
3 Months -
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
1 Year Plan
Full Access Subscription
$538.47
$
338
98
1 Year -
Access to full question bank
-
Access to all flashcards
-
Access to all chapters & site content
Popular
Loading table of contents...
Loading table of contents...